Adoptive cell therapy has gone on to become a promising immunotherapy tool that can be used to help in the treatment of advanced melanoma. The therapy, which makes use of the immune cells that are collected from the individual’s own tumours, can go on to provide new treatment options to cancer patients, thereby potentially bypassing cancer therapies and also those harsh chemotherapy drugs.
For the very first time in history, the Northwestern University scientists have explored whether it is indeed possible to isolate the tumour’s attack cells non-invasively via blood rather than from the tumours. These findings thereby open the door for the ACT to take care of the harder-to-reach cancer types, thereby making it a more viable option when it comes to hospitals.
As per Shana O. Kelley, paper’s corresponding author, they had begun probing about whether the immune cells which enter the tumours come back out and if one could find them in the bloodstream. She added that they did not know if they would be able to find them or see enough of them so as to even study them. Apparently, this is the first time these cells have been examined in this very context.
The study that is published in the Nature Biomedical Engineering journal is a continuation of the previous work that was done in the lab, which was again published in the same journal. In the previous study, Kelley as well as her team had gone on to treat the mice through their own immune cells, which were gathered from a mass, which most importantly shrank their tumours compared to traditional cell therapy methods.
The paper, which was published last year, also laid out a detailed method that is used to isolate as well as multiply tumour-infiltrating lymphocytes, a process that goes through and harvest cells to gain more than what the current approaches are giving, thereby making the anti-cancer response much stronger.
By removing and processing the melanoma tumours, the scientists have found TILs in them. That said, at times, removing the tumours so as to harvest TILs can prove to be a bigger risk to patients, leaving no gap to harness ACT so as to fight many cancers. Post finding TIL-like lymphocytes in the animal blood, the team went on to test whether or not cTRLs had the same capacity as TILs to thwart the tumour cells, and surprisingly, they did.
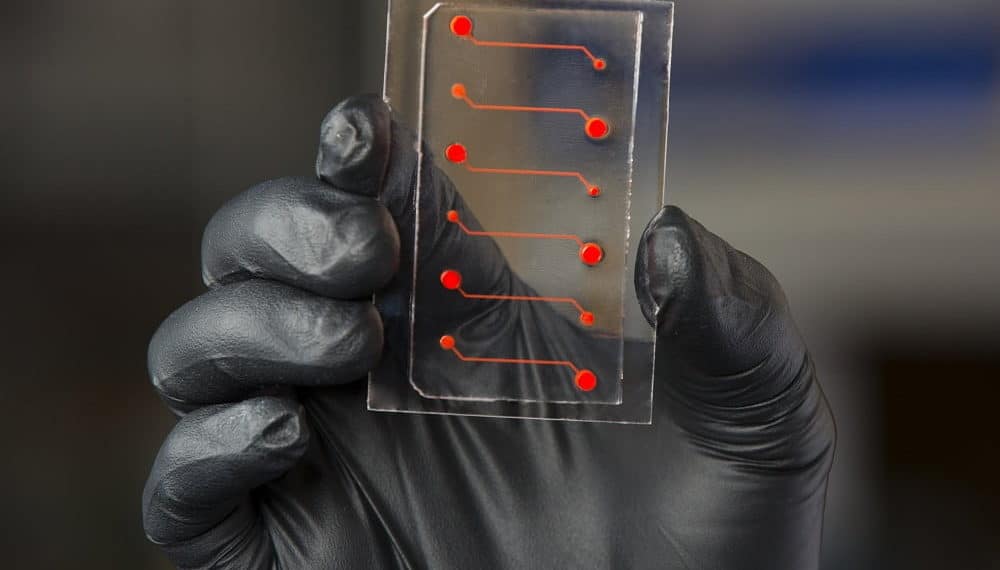
To get over another point, post-finding as well as profiling cTRLs, Kelley also used its new technology platform in order to isolate and then also replicate only those tumour fighters that were best.
It was seen that the cTRLs efficiently again levelled competition by engaging in a direct combat with the tumour cells. Kelley goes on to add that the engineering-based tools enable doing things that open up new biological regions. As per her, they could see making use of the platform across any major medical centre so that a significant number of patients could be reached. The platform that they used to capture the cells is very fast, thereby helping to bring the costs down, and besides, medical centres happen to be comfortable handling blood.
It is well to note that the scientists also found the cTRLs not only in melanoma models but also in breast, colon, and lung cancer, where each tumour represented a distinctive signature that TIL gets bound to.