Since 2019, the SARS-CoV-2 that produces COVID-19 has tragically highlighted the fragility of humanity to new coronaviruses by killing 6.3 million people globally.
In order to combat SARS-CoV-2 and all of its potentially dangerous variations, namely Beta, Gamma, Delta, Epsilon, and Omicron, researchers have discovered a neutralising monoclonal antibody. The deadly prior coronaviruses, SARS-CoV, the Severe Acute Respiratory Syndrome, which appeared in China in 2002, and MERS-CoV, the Middle East Respiratory Syndrome, which appeared in Saudi Arabia in 2012, also demonstrate its efficacy against them. Even against a few coronaviruses that cause the common cold, it exhibits potency.
The S2 stalk region of the viral spike (S) protein, which is structurally similar among beta-coronaviruses but also necessary for the virus to adhere and enter cells, is the target of a monoclonal antibody that has universal effectiveness against all beta-coronaviruses. In tests on animals, the monoclonal antibody offered protection from infections when given orally or intraperitoneally. James J. Kobie, Ph.D., Luis Martinez-Sobrido, Ph.D., of the Texas Biomedical Research Institute, San Antonio, Texas, and Mark R. Walter, Ph.D., of the University of Alabama at Birmingham, are co-senior researchers of the study that was published in the journal PLOS Pathogens.
Under licence to Aridis Pharmaceuticals, a California-based biopharmaceutical business, the monoclonal antibody and another monoclonal antibody revealed earlier by the researchers are being investigated as a treatment cocktail for COVID-19. Finding antibodies that prevent immunological escape by mutant versions of SARS-CoV-2, the virus that causes COVID-19, is the main objective of scientists at UAB, Texas Biomedical Research Institute, and Aridis. Omicron and any foreseeable variations of concern are included in this. It is believed that locating and researching these antibodies may result in the creation of vaccinations that offer protection against all coronaviruses.
According to Kobie, SARS-CoV-2 represents the third time a beta-coronavirus has significantly increased human mortality in the last two decades. Most illnesses and fatalities globally have been brought on by SARS-CoV-2. Even in those who have received vaccinations or have already contracted the disease, new variants run the danger of escaping the immune system, and there is still a chance that in the future, other genetically unique coronaviruses will develop into new pandemic strains.
For these reasons, developing novel therapeutic and preventative medications as well as vaccine techniques with global activity against the coronavirus is crucial to protecting humanity against pandemics or breakouts of beta-coronavirus in the present and future. The receptor-binding domain, or RBD, which is found at the heads of the S viral protein spike that sticks from the surface of the virus, has attracted a lot of attention from immunizations and other monoclonal antibodies against SARS-CoV-2. There are 24 to 40 spikes per virus. Although the RBD is particularly effective at inducing an immunological response, that part of the S allows for several alterations that could enable the virus to evade antibodies.
The discovery of an antibody site on the S2, or stalk region, of the spike was crucial to the current research. Since changing it would interfere with its crucial function, this area is extremely conserved and only rarely mutates. The S2 stalk functions to introduce the coronavirus inside the target cell after the RBD at the head of the S binds it to a specific receptor on the surface of the target cell. The virus multiplies there, destroying the cell and unleashing a large number of fresh, contagious virions.
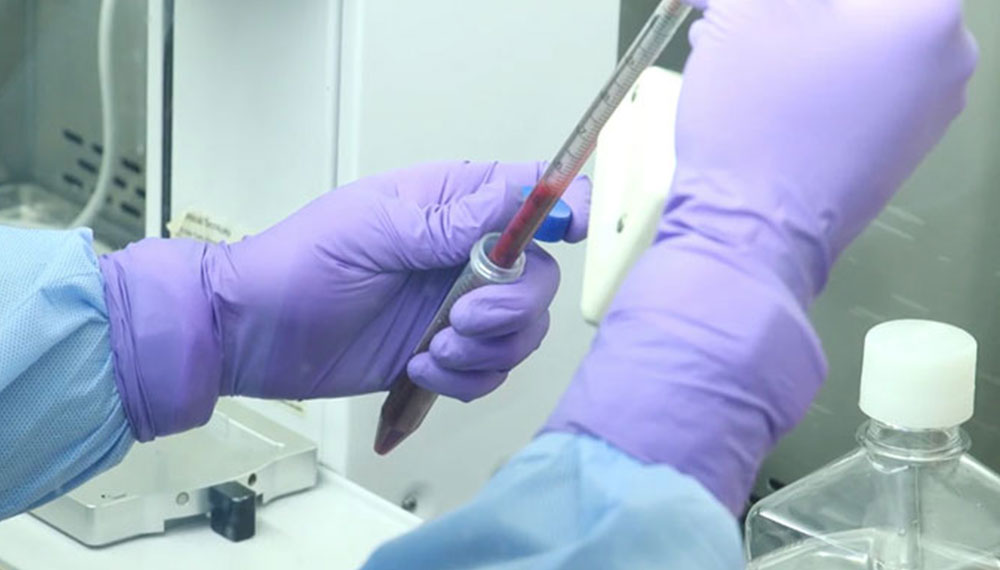
In order to find beneficial antibodies, Paul Goepfert, M.D., and Nathaniel Erdmann, M.D., Ph.D., of the UAB Division of Infectious Diseases, screened samples of blood from adult convalescent patients at UAB Hospital using the UAB COVID Enterprise Biorepository. Walter developed a panel of special cells capable of producing human monoclonal antibodies, or hmAbs, from memory B cells in the blood that were linked to custom S2 protein baits to simulate the normal state of the S2 domain of spike. These hmAbs were then evaluated for efficacy against the virus. Due to the immunodominant RBD, which is responsible for 90% of the convalescent plasma’s neutralising action, memory cells that target S2 are rare.
17 hmAbs demonstrated interaction with the S2 protein. Only four of these, including the Beta and Omicron varieties, were able to neutralise a SARS-CoV-2 pseudovirus and a live SARS-CoV-2. The best-performing antibody, the 1249A8 hmAb, showed the broadest and strongest neutralising effect against strains like the original SARS-CoV-2 from Wuhan, China, as well as the Beta, Gamma, Delta, Epsilon, and Omicron variations, the SARS-CoV and MERS-CoV, and two common cold viruses.
According to the maintenance of body weight and the removal of the virus from the mouse lungs 4 days after infection, the hmAb shielded mice from SARS-CoV-2 sickness. Furthermore, when combined with the researchers’ second newly found hmAb, 1213H7, the 1249A8 hmAb demonstrated synergism. Inhibitory to the viral S glycoprotein’s RBD is 1213H7.
The researchers have previously shown that straightforward respiratory delivery of a SARS-CoV-2 RBD-specific 1213H7 hmAb enables significant dose-sparing therapeutic activity in hamsters. This work was done in collaboration with Aridis, a company that specialises in the respiratory shipping of monoclonal antibodies to treat infections. Thus, using the S2-specific 1249A8 hmAb and the 1213H7 hmAb to treat SARS-CoV-2 and SARS-CoV, the researchers assessed this delivery method. The 1249A8, 1213H7 cocktail demonstrated a wide range of therapeutic activity in hamsters when administered as a nasal dose 12 hours after infection with SARS-CoV-2 Delta or the initial SARS-CoV identified in 2002.
These findings indicate in vivo cooperativity between S1- and S2-specific neutralising hmAbs and that potent universal coronavirus neutralising mAbs with therapeutic potential can be stimulated in humans and can serve as the foundation for the formulation of universal coronavirus vaccines, according to Kobie. Many SARS-CoV-2 RBD-specific hmAbs have received clinical use approval. Unfortunately, a number of them—including the most recent Omicron—have lost relevance due to their incapacity to neutralise problematic variants, underscoring the dangerous potential of RBD-only based mAb therapies against coronaviruses. The two hmAbs are used by Aridis in its AR-701 combination for inhaled administration. When used on people, AR-701 is designed to have a long half-life, possibly extending a year or more.