A new weapon in the arsenal of cancer cells’ treatment resistance, according to a study conducted by the Garvan Institute of Medical Research, is their ability to respond randomly to chemotherapy.
Understanding why some tumour cells develop resistance to chemotherapy is a key issue in cancer research because it remains the main treatment for the majority of cancers.
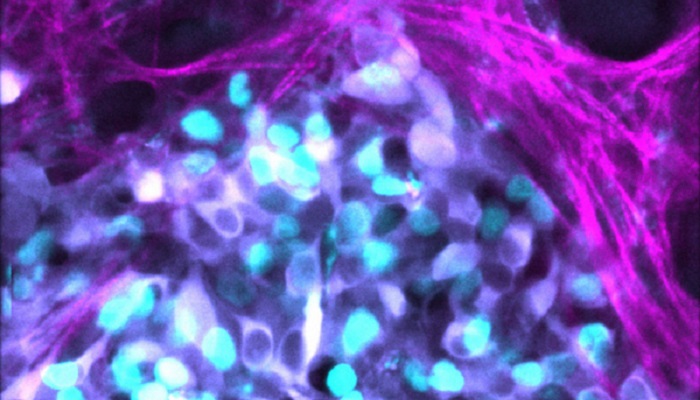
The latest study demonstrates that tumour cells from neuroblastoma, a malignancy that arises in the body’s sympathetic nervous system, can alternate between responding positively and negatively to chemotherapy.
Associate Professor David Croucher, director of the Network Biology Lab at Garvan, claims that noise is present in the process of cell death, which is precisely what occurs in chemotherapy resistance. This inherent noise, or randomization, in the system of gene expression, he claims, contributes significantly to this resistance.
Apparently, around 15% of neuroblastoma patients do not respond to the treatment.
According to Dr. Sharissa Latham, the co-lead author of the study, their results imply that genetics don’t account for everything; other layers of control and other mechanisms of cancer progression can also explain why we must investigate their pharmaceutical response.
The researchers demonstrated that neuroblastoma cells cannot reverse their resistance to chemotherapy once they have achieved it, indicating that there is only a small window of time for treatment to be effective on a tumour cell before it becomes locked in.
As a first-line therapy following a diagnosis and before tumors develop a condition of resistance, Associate Professor Croucher believes that chemotherapy combined with medications that target this cacophony within tumors may produce the best outcomes. This is the opposite of the standard cancer clinical trial strategy, where patients who have tried every other form of treatment are given a new one.
Science Advances is the journal where the new study has been published.
The researchers used mathematical modelling to filter out noise signals in the neuroblastoma tumors’ cell death pathways. Then, researchers applied it to patient cell samples, examining individual cells in sizable groups to spot those that did not visually respond to therapy.
In the process, they found a marker for resistance, which happened to be a set of proteins that were involved in the cell death process, also known as apoptosis.
They were seeking to understand the source of that randomness. Dr. Latham questions what it is about those cells and whether anything can be done to get them to react.
To stabilize the expression of the genes involved in cell death or by altering the inherent threshold that may tip a cancer cell into a resistant state, the researchers discovered specific types of licensed medications that may be used with chemotherapy.
The work will now begin to advance to a clinical study.